Labour & Delivery

- Hypnobirthing is a method of pain management that can be used during labour and birth. It involves using a mixture of visualisation, relaxation and deep breathing techniques.
- Childbirth delivery options include natural unassisted childbirth, assisted childbirth, and delivery by Cesarean surgery (C-section). Childbirth delivery locations include at home, in a birth center, or in a hospital.
Here in the UK You choose how & where you want to deliver your baby (as long as you are low risk). You can change your mind at any time during your pregnancy. In Bristol local choices include:
Weston General Hospital
Ashcombe Birth Centre
North Bristol NHS Trust
Cossham Hospital Birth Centre
Southmead Hospital central delivery suite
Southmead Hospital birth suite
University Hospitals Bristol
St Michael’s Hospital

🙋🏼♀️First time Parents
👶🏼Known baby boy
❤️Romeo
🍾Spontaneous labour (40+3)
⏰ Born on 20.08.20 @ 01:39 AM
⚖️ 4204 kg
🏥 Bristol Southmead Hospital – unplanned forceps delivery in a theatre
➡️ Triggers: quite a big baby & polyhydramnios
🏥Born during pandemic
💊 No pain relief / spinal in the theatre
🔸 Tearing: Episiotomy; Labial laceration
🔸 Total 5 days in a hospital: examination of the newborn; IV antibiotics
✨ Ain’t easy, but absolutely positive birth experience, happy adorable baby & happy parents.
I & my husband moved from London to Bristol a year ago (spring-summer 2019). We really wanted to start a new stress free life & have a baby in a calmer environment.

Both artists (music / video & photography) found Bristol as a great place to fit all our needs. Taking so many changes in our lives into account, we were not expecting to get pregnant quickly, but it happened as soon as we tried.
Being pregnant during covid-19 was extra challenging. On top of morning sickness, baby brain, frequent urination & increased hormones I also was diagnosed with meralgia parasthetica (numbness & burning pain in thighs) when i was 13 weeks. Since then i was mainly sleeping in a pretty much sitting position, because it’s not recommended sleeping on your back. I was waking up early and few times at night due to uncomfortable sleeping & achy lower back, however at the same time was able to watch beautiful sun rises. Covid made it difficult to manage the pregnancy with no swimming pools open, physio over the phone & continuous anxiety. Hospital tours cancelled, midwife appointments over the phone & lack information.
* Experts recommend pregnant women avoid sleeping on their backs during the second and third trimesters could cause stillbirth.
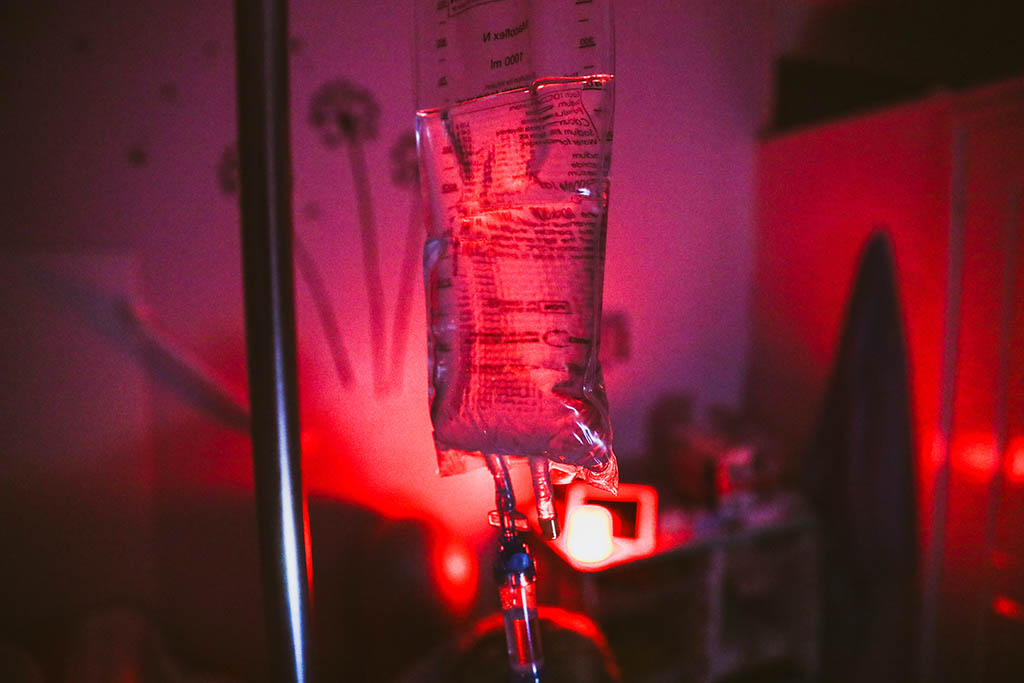
Being a curious & knowledge hungry person I struggled a lot with the lack of information. I really wanted to be prepared for the birth & my postpartum period. At the same time i heard about not getting enough knowledge & information from other girls before covid, so i felt i was getting even less. I started researching online & joining different zoom calls. And this is when i came across Positive Birth Company free workshop. It was my 28th week. I & my husband joined youtube stream that Siobhan did & we just loved it. It was very informative & positive, exactly our type of learning style. My husband purchased me a digital pack straight after that call. I never considered a birth centre or home birth before, but after the course i changed my mind completely & we decided to go for a Mendip Birth Centre (midwife-led Unit situated along the corridor from the Central Delivery Suite at Southmead Hospital ). I started practicing breathing technics every day. Our master bathroom became my cave with lots of candles & essential oils i loved. All my number 2s were breathed out in a calm red light environment. Breathing & Freya app helped me to manage the episode of very strong surges during week 30, which i though was potentially a labour as it was very strong & lasted for 4 hours, but it was fake – Braxton hicks. I purchased an essential oil diffuser which i used every day to build up the atmosphere i wanted for my childbirth. It helped me a lot and we used it for the actual labour too.
Last weeks of pregnancy were quite tough. During my 35 & 36 weeks midwives could not find baby’s head & one was quite sure he was breech, so i was sent for an additional scan. What a stress! Midwives should never assume & use the wording like “i think/i am quite sure”. I got a referral for a scan but they wanted me to wait until I turned 37 weeks & i knew why. 37 weeks is considered as a full-term & I think they wanted to offer me ECV (external cephalic version) which i knew i didn’t want to consent for until i tried other options like spinning babies or acupuncture. I called hospital few times pushing for the scan to be moved to an earlier date & 3rd time i called they moved it to the next day. Eventually Baby’s head was super low down, this is why it was hard to find it & even measure. It was a good sign & low chance to have a breech baby (babies can actually twist & change position until they are out). Our baby was preparing to see this world soon.
From week 37 I had a lot of body changes which made me feel that the miracle was going to happen soon. My feet, knees & fingers started swelling & every week the swelling was getting worse, my bump was big & growing & it was quite difficult to stay mobile. Skin around my belly button became shiny. I also had some period pains and belly tightening, so I felt I was ready to go into labour any time. I started thinking about how much i feel ladies that go for a sweep or stretch or an induction, but i really didn’t want to do it. My due date was 17.08.20. From the 16th I started getting continuous dull pain in lower abdomen and odd sensations. When i called the hospital they advised me to come to the Assessment Unit if this would have continued. On the 17th we went there for a check up. Monitors were showing good baby movements & contractions every 10 mins. I was 1-2 cm dilated, but i didn’t really have any surges. Doctor that examined me was not sure why i did have that dull constant period pain & offered to break my waters, however i refused. Taking my decision into account he asked for a second opinion from his boss and we were eventually ok to go home.

Later that day i started having a stronger sensations which seemed surges to me. It’s so hard to tell when it’s your first time. I called the Birth Center & they invited us to come. We arrived at the Birth Center, where the room was ready for us. As soon as i saw the midwife & her communication style i was 🤦🏼♀️ I felt like i was back in the USSR. First thing she asked was “where are you from?” When i said that i am originally from Estonia, she said she doesn’t speak Estonian, but we speak perfectly English. Honestly i really don’t get how can you start a conversation with this question by only looking at people. Then she looked at me & said that we would have to go to a delivery suite for further monitoring without literally explaining anything. And her style of communication was so patronising. All my sensations & surges were gone! I was extremely unhappy & just wanted to go home, but it was a start of the nightmare. I was on monitors for some time & that midwife kept on commenting how big my belly was – bump and a half she kept on saying. When she asked about the gender of my baby & i said it’s a boy, she literally said “ oh my Gosh” & left the room. That was absolutely ridiculous! After some time 2 doctors examined me & did scans (i asked for 2 opinions) & they both told me that i had an excessive amount of amniotic fluid & they both recommended to break my waters, but i used my BRAIN, asked a million of questions & then declined. I knew that if they broke my waters, my contractions could not have started because i had zero oxytocin & i needed to recharge. Midwife said that i was not going home for sure & should have stayed in a hospital labour ward to avoid any risks. This was a disaster for me, as i just generally don’t like the ward environment – being surrounded by random people. Partners were not allowed to stay due to covid. I started crying. All i wanted was to leave the hospital. We then had a discussion with my husband, collected all necessary info about potential risks, which were mainly around prolapsed umbilical cord, and took a decision to leave.
I was discharged against medical advice around 2AM on the 18th, but i knew it was the right thing for me to do. I was also offered an additional, more sophisticated, scan as they said at the Antenatal Unit. I got an appointment for the 19th at 9AM. I had a full day to recharge & get my oxytocin back. Our scan went really well. Sonographer was very reassuring & did say that my amniotic fluid amount was just within the limit at the edge, but she also added that bigger babies have more fluid and it’s absolutely normal. She was really nice & friendly & i felt myself in good hands. I also then had a chat with another doctor (3rd opinion), who was just amazing. She did recommend me to book an induction for the next day, but not necessarily go for it. Booking was necessary just to stay in the queue. Her concern was around my pains and the size of my baby(4+kg). She advised me to go home, detach, relax & try to forget about being pregnant as much as it was possible. She also advised i could postpone the induction & just continue with the monitoring. She was not pushy at all comparing to doctors from the night before & respected my choices. She was very supportive & made me feel really comfortable & relaxed. We went home. Due to swelling I had my legs lifted in a car & on my way out of the car, before even entering our house, i felt a little click inside. My waters started breaking gradually as soon as I stepped in to our flat. It was 13:37 & it took about 30-40 minutes for few chunks of waters to come out. I and my husband were so happy and excited. Oxytocin was literally flowing all over.

In about half an hour i started having very strong surges & they progressed extremely quick. When we were in the hospital earlier that morning we were advised to get straight back if my waters would break. I called the Assessment Unit and informed that we were coming back. When we arrived to the hospital i was no longer mobile. My surges were 1-3 mins apart. My tears were splashing out of my eyes, simply because surges were so strong & i could not control anything. Up breathing was literally impossible, so i switched to down breathing. Hospital was overcrowded due to power incident in St Michael’s Hospital. I had to wait for some time in the Assessment Unit for our room to be prepared. My husband was in the other part of the building as he was not allowed in the Assessment Unit. Separation was terrible. All I wanted was him to be by side holding my hand. At around 16:45 i was taken to a Delivery Suite where we finally met & i was examined & confirmed i was 7-8 cm dilated. I requested a different room with the pool. I really felt like being in a water. We had to wait for a little while again and after some time we got in to the nice room & I finally entered the pool with nice & warm water. My husband decorated the room nicely, turned my playlists on & this is how our journey began.
I liked being in a water, it was helping a lot. However midwives advised to be out from the pool for delivery stage. We were listening to my “labor” playlists, my husband was feeding me with some soya chocolate yoghurt & was keeping my hydration and energy levels up. I had lots of water and 5 bottles of Lucozade. I felt like everything was going quick. By 9 PM i was fully dilated. Midwives expected to see the baby shortly, but unfortunately, after actively pushing for 2 hours using different positions and techniques it did not happen. I was offered to be relocated in to another room with a gynaecological chair where doctor examined me & helped to empty my bladder as it was 1 L full. By that time I was extremely tired, but was still ready to continue pushing. Eventually they told me that it looked like the baby stuck & to avoid any stress + further risks for both of us it was best to action & try assisted delivery before it was turning into an emergency. I was completely agree with the recommendation & gave my consent for forceps delivery & c-section should that had become necessary. I was advised to stop pushing during surges & was actually happy to stop. All I was waiting for was the spinal (anaesthetic) to finally relax, have some rest & deliver my baby.
As soon as the theatre was free i & my husband were transferred there. Eventually both doctors, who examined me & suggested to break my waters 2 nights before, were helping to deliver my baby. Funny enough one doctor approached me and asked: “Do you remember me?” and I was “NOOOOO, not you” – joking. They did a really good job.. I was happy with the forceps delivery decision they took & not a c-section. Everything happened very quick & our baby boy Romeo was born at 01:39 AM on the 20th of August 2020. Total (1st, 2nd & 3rd stages) labour duration was 9h 10mins. Both i & my other half think that all went really well & we used our BRAIN to take right decisions at all times. Absolutely positive birth experience thanks to the digital pack. If we did not have the knowledge & technics we learned from the course we would not have coped the way we did😎💪🏼
I will write a separate article about my hospital bag, our 5 never ending days in the hospital after birth & postpartum period. Stay tuned!
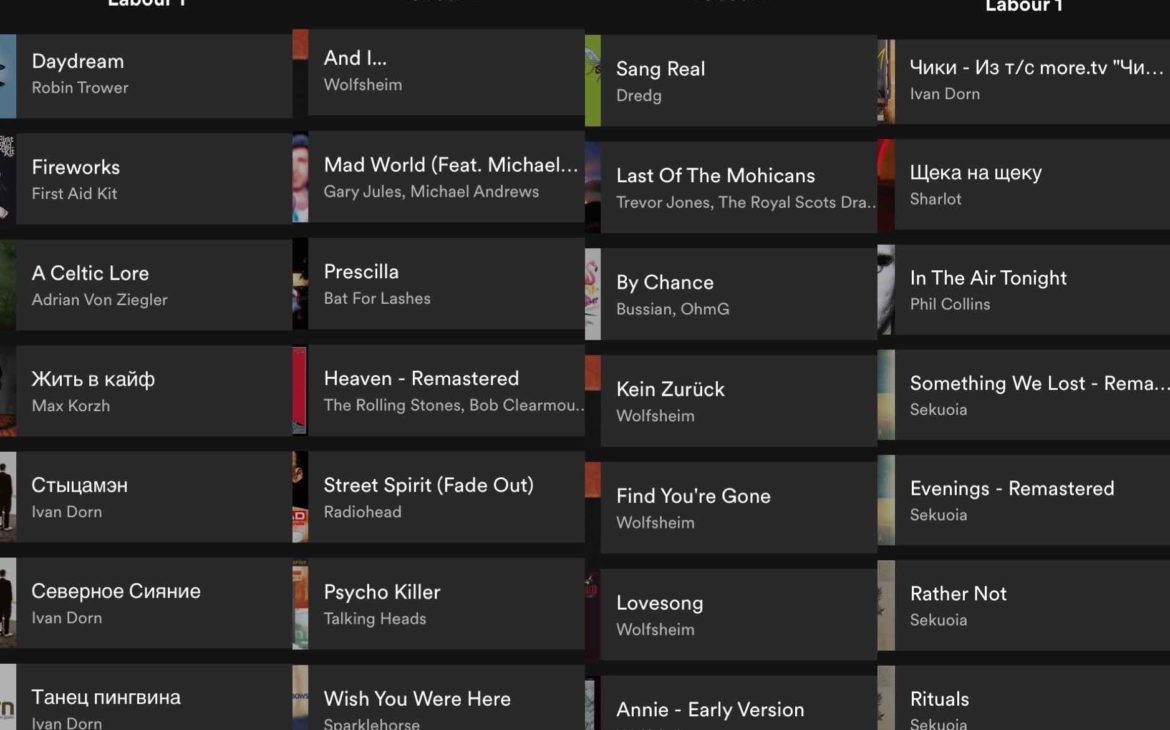
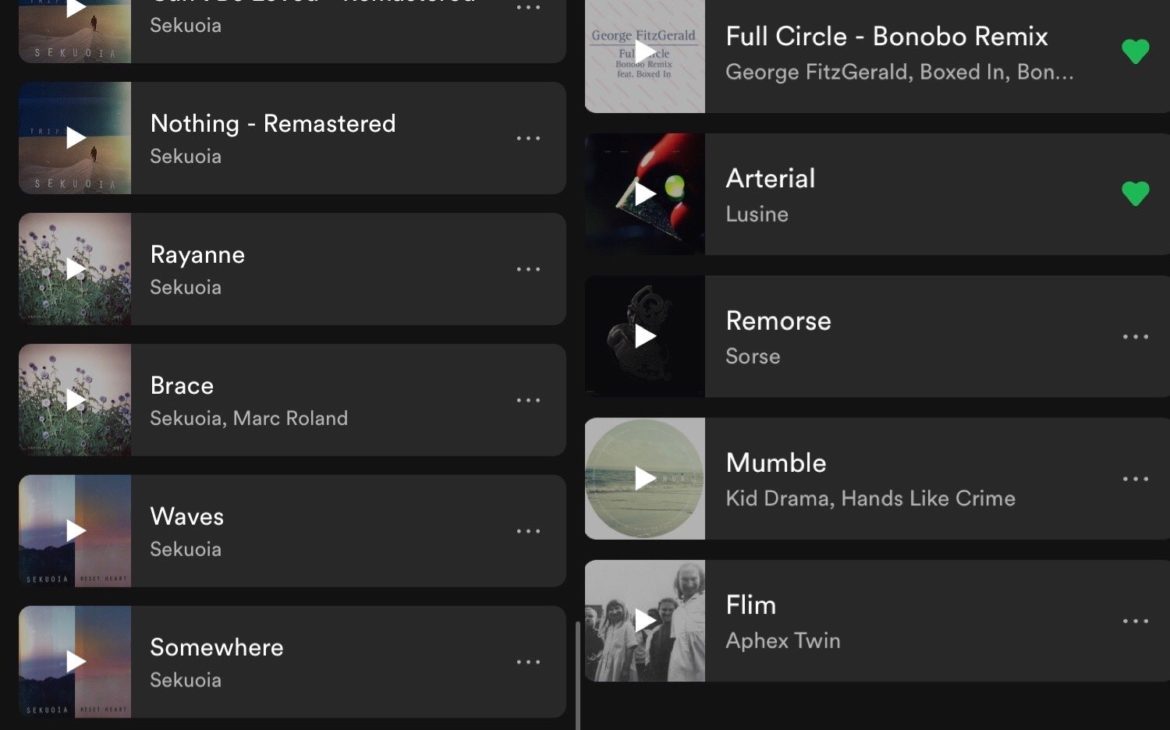
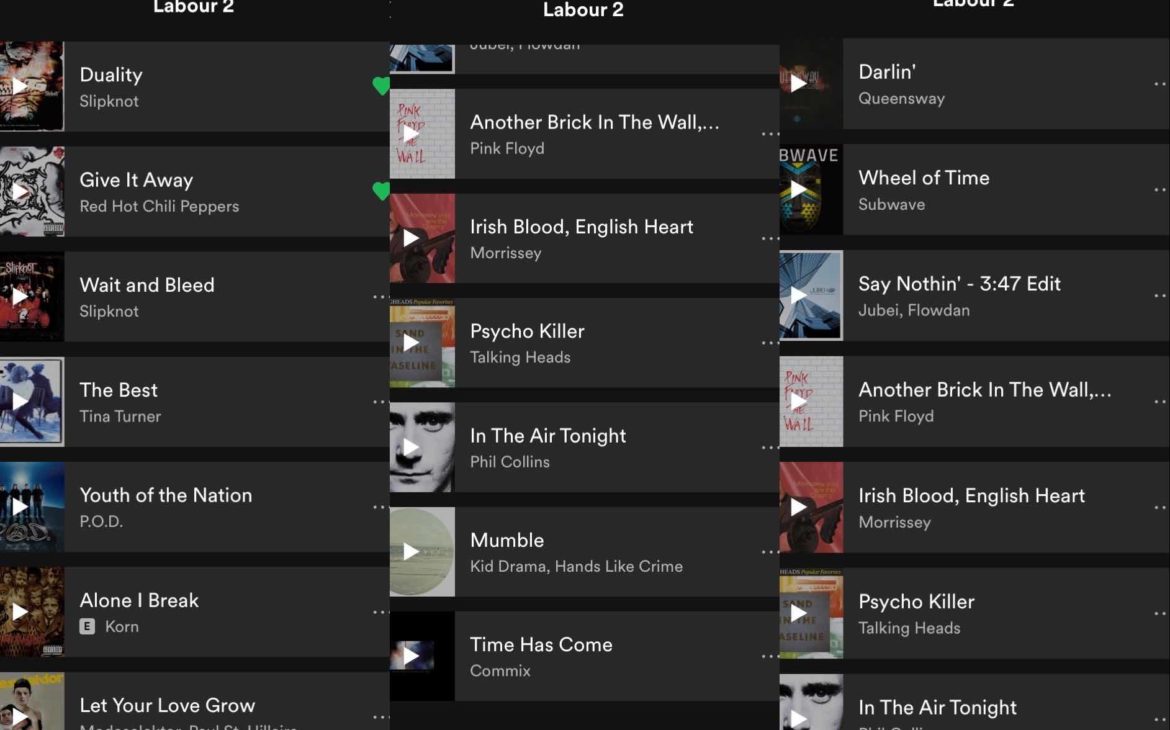
My Labour playlists for 2 stages.
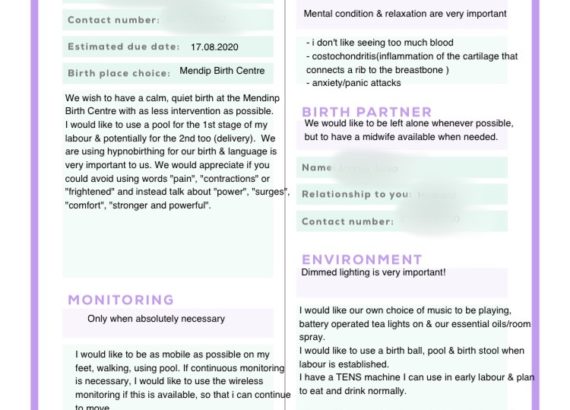
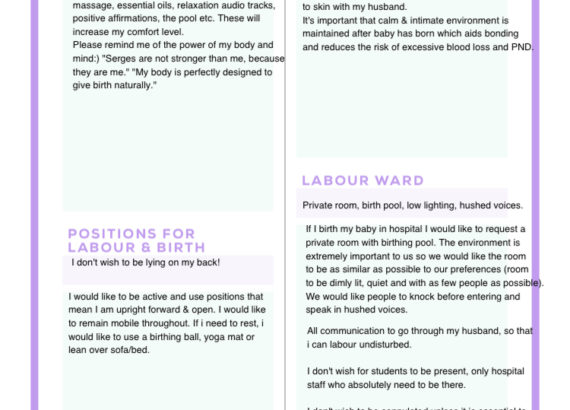
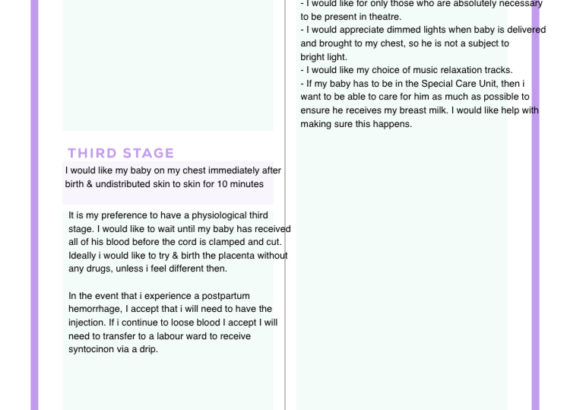
My birth preferences:
Useful links & organisations you can trust:
LULLABY TRUST
LA LECHE LEAGUE GB
THE POSITIVE BIRTH COMPANY
(These guys constantly do discounts, so i would recommend you to subscribe).
Apps i used & continue using:
YogiBirth ( pregnancy yoga, meditation, education).
Freya (breathing technics & positive affirmations)
Special THANKS goes to Joanne Arkwright ( 3rd opinion doctor), Catherine Walker, team who worked in the theatre & my husband, who actively participated in our child birth and was told he could join the midwifery team now:)